Discharge Instructions: Blood Transfusions for Children
Understanding blood and blood parts
Your child has recently had a blood transfusion. A blood transfusion may be done when your child has lost blood because of an injury or during surgery. It can also be done because of diseases or conditions that affect the blood.
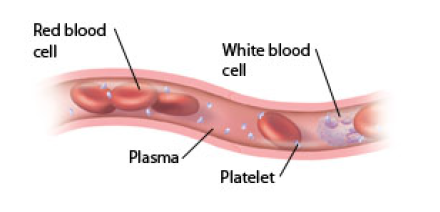
Blood is made up of many parts, called blood parts. These include red blood cells, platelets, and plasma. Your child has received some of these blood products during their transfusion. Blood used for transfusions is often donated by another person (donor).
The parts of blood
Blood can be separated into different parts that perform special roles in the body. These parts include:
1. Red blood cells (RBC), which carry oxygen throughout the body
2. Platelets, which help stop bleeding
3. Plasma (the liquid part of blood), which carries red blood cells and platelets (and white blood cells) throughout the body. Plasma also contains proteins like clotting factors that help stop bleeding.
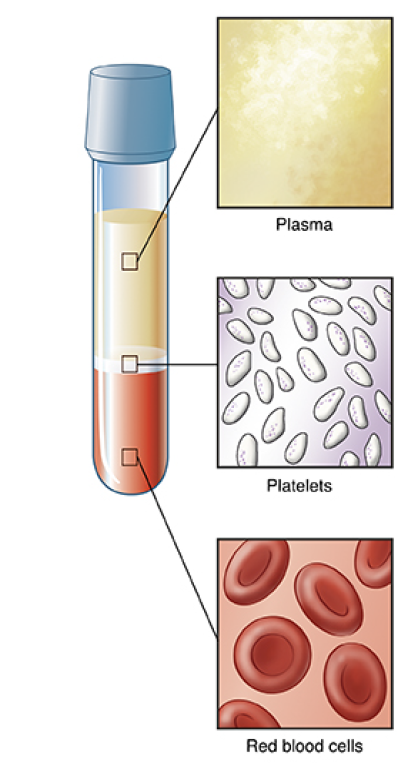
Blood can be separated into three parts,
which include plasma, platelets, and red blood cells.
Are blood transfusions safe?
Donated blood is tested and processed to make sure that it's safe:
• Donor screening. The health and medical history of each donor is carefully screened. If a person is considered high-risk for infection or problems, they aren't accepted as a donor.
• Infection testing. Donated blood is tested for infections such as hepatitis, syphilis, West Nile virus, human T-lymphotropic virus, and HIV (the virus that causes AIDS). If the tested blood is unsafe, it is not used for transfusion and not given to another person.
• Blood types. Blood is grouped into four types: A, B, AB, and O. Blood also has Rh types: positive (+) and negative (-). A sample of your child’s blood is tested for compatibility with donated blood. This is done before blood products are prepared for a transfusion. Your child can only get blood products that match their blood type unless it is an emergency.
• Emergency situations. In emergency situations where there isn't time to find out your child’s blood type, they may receive universal red blood cells or whole blood from blood type O donors, as well as plasma from donors with blood type AB or A.
What is directed donation?
Directed blood donation is a donation by a family member or friend for a specific patient. This option is not often recommended. Donated blood is very carefully tested and safe for transfusion.
Studies have shown that standard blood donations are just as safe, if not safer, than directed donations. However, if you have concerns, you may discuss them with your child’s doctor. In cases where a doctor determines that a directed donation is medically necessary, arrangements can be made.
How is a blood transfusion done?
A blood transfusion often takes place in an infusion center, at a patient’s bedside, or in an operating room. Your child’s doctor will discuss the blood transfusion with you before it’s done. You’ll need to give permission for the blood transfusion by signing a consent form.
-
Your doctor confirms your child’s identity. They also confirm that they have the correct blood products for your child.
-
An IV (intravenous) line is placed in a vein if they don't already have an IV. This may cause your child some brief discomfort. Your child may be given medicines before the transfusion to prevent transfusion reactions.
-
The blood product comes in a plastic bag that is hung on an IV pole. The blood product flows from the bag into your child’s IV line. The IV line is connected to a pump, which controls the transfusion rate. Your child may get more than one kind of blood product through the IV.
-
Your child’s blood pressure, heart rate, respiratory rate, and temperature are checked throughout the transfusion. This is to make sure they are not having a reaction to the blood product.
-
How long the transfusion takes depends on the type of blood product, the amount in the bag, and how well your child tolerates the transfusion.
-
The IV line may be removed once the transfusion is complete.
Possible risks and complications of a blood transfusion
Most transfusions are problem-free. But reactions may happen. Most reactions are mild. In rare cases, serious and life-threatening reactions occur. These can happen within minutes or hours after the transfusion is started or even a week to a month after the transfusion.
The most common reactions from blood transfusions are mild allergic reaction and fever. Call the doctor right away or get medical care right away if your child has any of the signs and symptoms after a transfusion. The signs and symptoms are listed below under “When to seek medical care”. In some cases, you may be advised to bring your child to the nearest emergency room.
Home care
-
Your child will likely have a bandage over the transfusion site. Keep it dry and remove it as advised by their doctor.
-
After you remove the bandage, keep the transfusion site clean. To do this, wash your child's skin with clean, running water and mild soap. Gently pat it dry.
Follow up
Follow up with your child's doctor, or as advised.
When to seek medical care
Most transfusions are problem free. In some cases, reactions occur. Most are mild. Rarely, serious and life-threatening reactions occur. These can happen within seconds to minutes during the transfusion or a week to a month after the transfusion. Call your child’s doctor right away if you have any of the symptoms below:
-
Fever 100.4°F (38°C) or as advised by your child’s doctor
-
-
Pain at your child’s IV injection site
-
Purple spots on the skin, hives, or itching
-
Swelling of feet or ankles
-
-
Cough, breathing difficulty or shortness of breath
-
Call 911
Call 911 if you have any of the following:
-
Trouble breathing, shortness of breath, wheezing, or chest tightness
-
Swelling of the lips, tongue, or throat
-
Chest, back, or belly pain
-
-
Fainting, dizziness, or loss of consciousness
-
Fast (rapid) heart rate or pulse