Preventing Venous Thromboembolism (VTE) in the Hospital
Health care providers use the term venous thromboembolism (VTE) to describe two conditions, deep vein thrombosis (DVT) and pulmonary embolism (PE). They use the term VTE because the two conditions are very closely related. And, because their prevention and treatment are closely related.
DVT is a blood clot or thrombus in a deep vein. Most of these clots develop in the leg or thigh. But, one may form in a vein in the arm or other parts of the body.
Part of the blood clot may separate from the vein. This is called an embolus. It may travel to the lungs and form a pulmonary embolus. This can cut off the flow of blood. A blood clot in the lungs is a medical emergency and may cause death.
This handout provides information on the risk factors for and how to prevent DVT and PE while you are in the hospital.
Risk factors for DVT and PE
Anyone can develop a blood clot. But the following risk factors make a blood clot more likely to occur:
-
Being inactive for a long period, such as when you’re in the hospital, or traveling by plane or car
-
Injury to a vein from an accident, a broken bone, or surgery
-
Having blood clots in the past or a family history of blood clots
-
Blood clotting disorder
-
Recent surgery
-
Cancer and certain cancer treatments
-
Smoking
Other factors can also put you at higher risk for a blood clot. They include:
-
Age over 60 years
-
Pregnancy
-
Taking birth control pills or hormone replacement
-
Having other vein problems, such as varicose veins
-
Being overweight
-
Having a pacemaker or a central venous catheter. They increase the chance of a blood clot forming in an arm.
-
Injection drug use. This also increases the chance of a blood clot forming in an arm.
Prevention of DVT and PE
Your health care provider will usually prescribe one or more of the following to prevent blood clots based on your risk.
-
Anticoagulant. This is the medicine that prevents blood clots. You take it by mouth, by injection, or through an IV. Commonly used anticoagulants include warfarin and heparin. Newer anticoagulants may also be used, including rivaroxaban, apixaban, dabigatran, and enoxaparin. Sometimes your health care provider may not give you an anticoagulant medicine. It is important that he or she discuss the risks and benefits with you, and document them.
-
Compression stockings. These are elastic stockings that fit tightly around your legs. They help keep blood flowing toward your heart by the pressure they apply. They prevent blood from pooling and forming blood clots. When you first put them on, the stockings may be uncomfortable. But after a while, you should get used to them.
-
Exercises. Simple exercises, while you are resting in bed or sitting in a chair, can help prevent blood clots. Move your feet in a circle or up and down. Do this 10 times an hour to improve circulation.
-
Ambulation (getting out of bed and walking). After surgery, a nurse will help you out of bed, as soon as you are able. Moving around improves circulation and helps prevent blood clots.
-
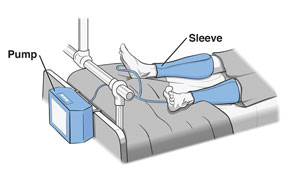
The sequential compression device (SCD) or intermittent pneumatic compression (IPC). Plastic sleeves are wrapped around your legs and connected to a pump that inflates and deflates the sleeves. This applies gentle pressure to promote blood flow in the legs and prevent blood clots. Remove the sleeves so that you do not trip or fall when you are walking. For example, when you use the bathroom or shower. If you need help removing the sleeves, ask the nurse or aide.